Given a combination of economic and political factors, HLA previously predicted an uptick in the frequency and intensity of pharmacy audits in 2024. Unfortunately, HLA's predictions appear to be spot-on, and the information we are receiving from clients indicates that PBMs are terminating network pharmacies based on minor and inconsequential audit violations at a higher rate than ever before. In addition, a late December 2023 announcement from the Department of Health & Human Services ("OIG"), confirms that the "feds" are now prioritizing pharmacy audit enforcement.
OIG Oversees the Medicare & Medicaid Programs
OIG is one of the largest federal agencies and is responsible for maximizing the efficiency of government healthcare programs. Among other responsibilities, OIG ensures the programs operate efficiently by policing fraud, waste and abuse, including the submission of false claims, kickbacks for referrals, medical identity theft, and abuse in nursing homes.
Each year, OIG establishes priority areas for enforcement, with certain probes conducted by the Office of Audit Services. These efforts are publicized in OIG's Work Plan, which is updated monthly. OIG focuses on those areas it believes are most in need of attention.
OIG's 2024 Work Plan Prioritizes Inventory Audits
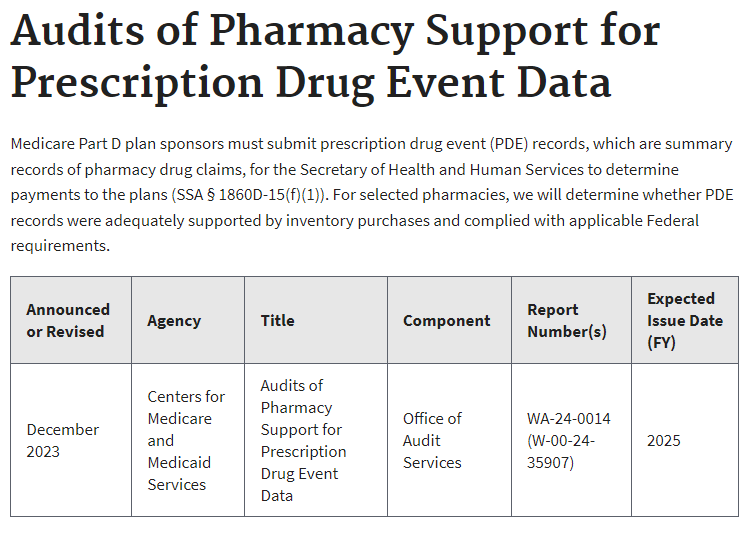
In December 2023, OIG updated its workplan to include "Audits of Pharmacy Support for Prescription Drug Event Data." When pharmacies submit claims for reimbursement, they are contained in a Prescription Drug Event (PDE) record that is relied on by the government and plan sponsors for adjudication. The PDE contains various data elements, including prescription drug costs and payment data that enables CMS to make Medicare and Medicaid payments.
Specifically, OIG announced that it will conduct audits to "determine whether PDE records were adequately supported by inventory purchases and complied with applicable Federal requirements." In other words, in addition to MCOs, PBMs, and CMS auditors, now a federal agency is planning to conduct inventory audits directly. Here is OIG's announcement:
Inventory Discrepancies are Mostly Trivial
HLA has published numerous articles on the defense of inventory audits, which you can access HERE and HERE. In summary, inventory shortfalls are commonplace due to the complexities of pharmacy practice. Accordingly, the federal government's focus on pharmacy inventory audits appears misguided.
For example, where is the compelling federal interest in whether a diabetic failed to pick-up his or her insulin? Or a patient had enough doses remaining on an inhaler to skip the refill? As a long-time, former public servant for the federal government, I always understood that the focus should be on the most meaningful and impactful issues. "Don't make a federal case out of it," is a saying for people blowing things out of proportion. Now, however, it seems the government is making a federal case out of trivial matters.
HLA Specializes in Audit Defense
Politics aside, the consequences of any type of failed audit can be severe, including recoupments, network sanctions, licensing board issues, and even criminal prosecution. Our experienced healthcare defense attorneys have a demonstrated track-record of highly successful outcomes in these cases, including the outright dismissal of criminal indictments and settlements for fractions of the claims paid with no licensing ramifications. Whether it be a PBM, payor, or OIG audit, our audit specialists are always available. Don't wait until your rights are jeopardized to pick up the phone.
MORE ARTICLES BY CATEGORY
The 2025 Healthcare Fraud Takedown Is a Warning Shot for Wound Care Providers
Wound care is now an enforcement priority. The 2025 fraud takedown targets skin substitute billing, graft utilization, and Medicare compliance.
Read More >>FDA and Novo’s Uncharted Waters to Exert Pressure on Hims & Hers and GLP-1 Compounders
Novo’s lawsuit against Hims & Hers, coupled with FDA’s referral to the DOJ, marks a direct escalation against 503A compounded semaglutide. If your pharmacy dispenses, compounds, or markets GLP-1 therapies, this is not a headline, it is a regulatory turning point.
Read More >>What Wells Pharma v. Zyla Life Sciences Means for Compounding Pharmacies and Outsourcing Facilities
A pending Supreme Court case could reshape how compounding pharmacies face litigation under state unfair competition laws tied to FDA approval standards.
Read More >>Health Law Alliance Welcomes Compounding Expert Pharmacist-Attorney Dr. Martha Rumore as Of Counsel
Health Law Alliance adds powerhouse Pharmacist/Attorney Dr. Martha Rumore to their team of boutique healthcare attorneys.
Read More >>